Huntington Disease
Huntington disease is an inherited degenerative brain disorder. It is caused by the inherited defective gene that damages certain nerve cells in the brain. Huntington disease or HD typically affects the person at three levels, physical, cognitive and psychological parameters. Thus the patient gradually loses the ability to move, think and feel efficiently. Though it is an inherited condition, normally symptoms start to surface between the ages of 30 and 50.
The symptoms of HD can be classified into three groups:
1. Problems with movement
2. Problems with cognition
3. Behavioral problems
Movement Disorders
Uncontrolled movements is one of the early symptoms of Huntington disease. As the disease progresses, patient may experience the following symptoms:
- Involuntary jerking of legs, arms, face and upper body(chorea)
- Abnormal eye movements
- Problems with speech and swallowing
- As the disease advances, impairments in voluntary movements are also experienced.
Cognition Disorders
Cognitive changes may affect the ability of a person to work and manage things for himself. Some of the cognitive capabilities that get severely affected are mentioned below:
- Short-term memory loss
- Difficulties in planning and organizing
- Difficulty in processing thought and expression
- Trouble learning new information.
Behavioral Problems
Behavioral changes of the Huntington disease are the most distressing and difficult to handle. Some of the behavioral disorders are listed below:
Depression
Anxiety, denial
Mood swings, apathy and aggression.
Repetition which also includes obsessive compulsive disorder(OCD)
Altered sexuality.
Diagnosis
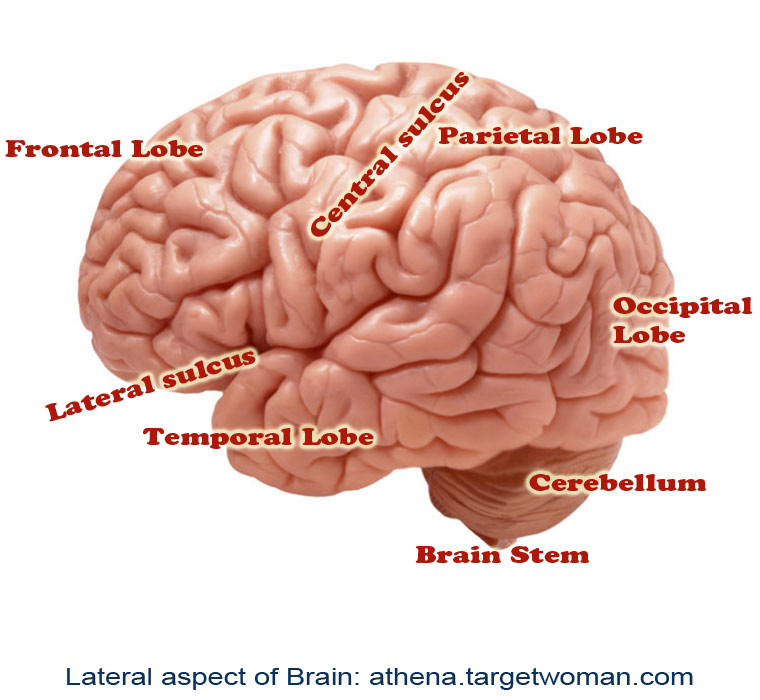
Thorough clinical examination and evaluating the history of the patients and parents is the first step towards diagnosing the condition. Imaging tests such as MRI or CT scan may also be advised to examine any structural changes in the brain. A diagnostic genetic test can confirm that the defective gene is responsible for Huntington disease.
Treatment
There is no cure for Huntington's disease, treatment is only directed towards controlling the clinical symptoms. Medications are advised over the course of the disease to control the symptoms of movement and psychiatric disorders. Tetra benzine drug, Anti psychotic drugs, such as haloperidol (Haldol) and chlorpromazine, antidepressants are prescribed to treat physical and psychological problems. Physical therapy and occupational therapy may also be advised to improve the general condition of the patient. A nutritious diet also goes a long way in managing a patient with Huntington disease.
Deep Brain Stimulation
Deep brain stimulation is a specialized neurosurgical treatment option for patients suffering from a special group of neurological disorders called 'Movement Disorders'. Deep Brain Stimulation or DBS is an advanced procedure performed by neurosurgeons for treating patients who cannot achieve optimal results through conventional medical therapy alone.
Neurophysiology of Movement Disorders
Movement disorders refer to conditions associated with changes in specific areas of the nervous system which results in abnormal involuntary movements, slow or reduced movements. The two main areas of the brain which are affected in movement disorders are the basal ganglia and the sub-thalamic nucleus. The disorders are classified into various groups such as hypokinetic disorders (e.g.: Parkinsons), hyperkinetic disorders (e.g.: Huntington's disease), and Non-motor disorders (e.g.: Tourette's Syndrome and Obsessive Compulsive Disorders). When these nuclei start having abnormal electrical activity (discharging too much or too little), the patient experiences specific symptoms related to movement.
Indications for Deep Brain Stimulation
Deep brain stimulation is used for patients who usually suffer from movement disorders such as Parkinsons, tremors, and dystonia. It is called Deep Brain Stimulation because surgically placed electrodes are used to stimulate specific areas (nuclei) deep inside the brain. The most common nuclei commonly stimulated are the Globus Pallidus and the sub-thalamic nuclei.
The idea behind DBS is that it functions somewhat like a 'pacemaker' in the brain, periodically sending electrical signals to the specific nuclei, thereby modulating the effect of these nuclei. Hence, DBS is also called as neuromodulation therapy'. In DBS, specific electrical signals are sent to the abnormally functioning nuclei to reduce or increase their activity.
Components
There are three components of the Deep Brain Stimulation system. They are:
The Stimulating Electrodes
The IPG – Internal Pulse Generator (the pacemaker)
The Extension - connecting leads between the Electrode and IPG.
The IPD contains a battery pack which has to be replaced every 4 years. The IPG is programmed by the neurologist based on the specific disease condition of the patient, and the placement of DBS requires regular follow-ups for programming the IPG based on the disease condition, if needed.
Procedure
Specialized Brain Mapping technology is used to locate the specific nuclei which are suspected to be abnormally functioning. These nuclei are the 'target area' for DBS. A specially designed stereotaxic frame is attached to the patient's head which provides a three-dimensional reference system for the patient's brain and enables the neurosurgeon to precisely locate the nuclei or track the electrode tip during placement.
The procedure normally takes up to three hours and is performed by a neurosurgeon specially trained in the procedure. The surgery is called awake craniotomy since the patient is awake during the entire duration of the procedure so that his neurological functions can be assessed in real-time to see the 'before and after' results due to the electrode placement. Following the placement of the electrodes, the IPGs are implanted either during the time of the surgery or later on. Each brain is unique, and hence the IPGs have to be specially programmed and the settings have to be specific for each patient. This is usually done about 2 weeks after the electrode placement.
Clinical Results
It is not exactly known how DBS functions, but there have been marked clinical improvements for patients with Parkinson's disease, tremors, and dystonia. Although a large percentage of patients report significant improvement after DBS surgery, there is no guarantee that DBS will help every patient with movement disorder.
Patients with Parkinson's report 60-80% improvement in tremor and slowness of movement. Patients on an average report 50% improvement in their walking and balance following DBS. Others with dyskinesia (involuntary movements) report more than 80% improvement following DBS.
Complications
Although DBS on the whole has proven safe and effective, there is a possible 2-3% risk of intra-cranial hemorrhage and meningitis due to leakage of cerebro-spinal fluid. There is a 15% chance of developing infection due to the placement of the electrodes. There is a possibility that seizures may occur, if the tip of the electrode migrates, thereby stimulating other areas of the brain. However such findings have not been reported until now.
Future of DBS
Besides movement disorders, DBS has been used to chronic pain, and currently possibilities of using DBS for other cognitive disorders such as severe depression, obsessive compulsive disorder, eating behavioral disorders and drug addiction, are underway.
CJD
This is a rare degenerative disease, a fatal brain disorder. One in every million worldwide is affected by Creutzfeldt Jakob disease which occurs about age 60, and about 90 percent of patients die within a year. Since first described in 1920, less than 1 percent of cases have acquired CJD.
Signs and symptoms
During the early stages of the disease failing memory, behavioral changes, lack of coordination and visual disturbances are exhibited. Impaired memory, judgment and thinking and insomnia, depression or unusual sensations are other symptoms. CJD may also cause fever or other flu-like symptoms. As the illness progresses, mental deterioration becomes severe. Involuntary movements, blindness and weakness of extremities are other symptoms.
Rapidly the disease progresses into dementia. Patients eventually lose the ability to move and speak and then enter a coma. Pneumonia and other infections may occur in these individuals and can lead to death. Some symptoms of CJD can be similar to Alzheimers or Huntington disease. CJD causes unique changes in brain tissue which can be seen at autopsy and the deterioration is more rapid than Alzheimer's disease or other types of dementia.
Major categories of CJD
Sporadic CJD: Here the disease appears even though the person may not exhibit any known risk factors. This is by far the most common type of CJD and 85 percent cases come under this category.
Variant CJD is caused by consuming meat from a cow that had Bovine Spongiform Encephalopathy (BSE) or mad cow disease, a prion disease similar to CJD. Strict controls have proved very effective since its discovery in 1996.
In hereditary CJD, the person has a family history of the disease and tests positive for a genetic mutation associated with CJD. About 5 to 10 percent of cases in the US are hereditary and the symptoms usually develop in early 50s.
In latrogenic CJD, the infection spreads from someone through medical or surgical treatment. A common instance of this is spread of CJD from someone with growth hormone treatment using human pituitary growth hormones extracted from deceased individuals who might have had CJD infection.
CJD is not contagious through casual contact with a CJD patient.
Causes
Researchers believe that an unusual slow virus or any other organism causes CJD. But they have never been able to isolate a virus or any organism in people with the disease. As the agent causing CJD has several characteristics other than known organisms such as bacteria and virus, it is difficult to destroy as it does not contain any genetic information in the form of nucleic acids. For example, prions are not destroyed by the extremes of heat and radiation used to kill bacteria and viruses, and antibiotics or antiviral medicines have no effect on them. It also incubates for a long period of time before the symptoms appear, as long as even 50 years. The leading scientific theory maintains that CJD is caused by a type of protein called as a prion.
Also 5 to 10 percent of CJD cases are inherited. These cases arise from a mutation, or change in the gene that controls formation of the normal prion protein.
Diagnosis of CJD
There is no single diagnostic test for CJD. First, all treatable forms of dementia are ruled out. A neurological examination is performed and consultation with other physicians is sought. Spinal tap, electroencephalogram, CT and MRI and brain scans can reveal characteristic patterns of brain degeneration that can help diagnose CJD.
For a confirmed diagnosis of CJD, brain autopsy is the only way. A neurosurgeon removes a small piece of tissue from the patient's brain and it is examined by a neuropathologist. The procedure may be dangerous as it does not always obtain tissue from the affected part of the brain. Brain biopsy is discouraged unless it is needed to rule out a treatable disorder. In autopsy, the whole brain is examined after death. Special surgical and disinfection procedures can minimize the risk. Scientists are working to develop laboratory tests for CJD.
As such there is no treatment or cure to control CJD. Studies are on to try a variety of drugs but none of the treatments have shown consistent benefits in humans. Treatment aims at alleviating symptoms and making the patient as comfortable as possible. Opiate drugs can help relieve pain. During later stages of the disease, changing person's position frequently can keep them comfortable and help prevent bed sores. A catheter is used to drain urine if bladder control is lost. Intravenous fluids and artificial feeding are also used.
Avoid spreading CJD
To reduce the very low risk of CJD transmission from one person to another, it is better not to donate blood, tissues or organs if suspected or confirmed with CJD because of family history of the disease. As normal sterilization procedures such as cooking, washing and boiling do not destroy prions, the following precautions are suggested by the World Health Organization while dealing with patients contacted with CJD.
- Cuts and abrasions should be covered with waterproof dressings.
- Surgical gloves should be worn when handling a patient's tissues and fluids or dressing up patient's wounds.
- Avoid cutting or sticking with instruments contaminated by patient's blood or tissues.
- Use disposable bedclothes for contact with patient.
- Use face protection if there is risk of splashing contaminated material such as blood or cerebrospinal fluid.
- Soak instruments that have come in contact with patient in undiluted chlorine bleach for an hour or more and then autoclave to sterilize them in distilled water for at least one hour at 132-134 C.
Tags: #Huntington Disease #Deep Brain Stimulation #CJD
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: February 24, 2026



